It’s been a while since you were here. It’s been a while since I was here. The last 5 posts were hard to get through, but I felt like I had to get them out not just for you who are reading this, but for myself – both as a way to remember and a way to express.
It’s not like nothing has been happening, though. Although as I reflect on what happened in that week of November, I felt like the world shook and when it was done, everything was in a slightly different place. Everything is off kilter. Nothing feels the same, but we are together and will face what comes together.
After we returned, we certainly felt like we needed a breather and to re-affirm life. Let’s say there were a lot of desserts eaten in the week after we returned from Boise.
The hospital made some referrals for us while we were in Boise for follow up visits and future treatments back in Seattle, but the appointments were a couple of weeks away from when we returned – that meant we had some time to recover from the emotional rollercoaster for a little bit.
In part 4, I mentioned that the tumor was a glioblastoma. After a few weeks, we got the detailed pathology report, and it came back as a “grade 4” glioblastoma with “hypermethylation” mutations… whatever that means. What I do know now, is that it is a very serious, fast-growing tumor, but one that responds well to a specific treatment regimen.
That regimen, unfortunately, is radiation and chemotherapy.
On December 11th, we sat through 5 back-to-back appointments in the Alvord Brain Tumor Center at Fred Hutch Cancer Center in the UW Medical Center in Seattle.
At this point, I was glad that I was not assigned to a project and that these visits did not interfere with my work – or my work did not interfere with these visits, which is probably more to the point.
Funny thing, though, was the day before, December 10th, I had just accepted an offer with a new company to start a new job at the end of the year (December 30th). Fortunately, they were able to get me on board in such a way to not interrupt our medical coverage – and not duplicate any deductible payments. So, that was definitely God’s timing – a new job, a 20% pay increase, and insurance starting January 1st.
(I’d tell you all about the job change process, but not now: this is a different story.)
Let me tell those of you who do not live in the Seattle area that the city is not well suited for commuting. We were not excited about having to drive into Seattle for treatment, but after conferring with the doctors, we were told that the best place to get treatment was there at UW Medical Center (UWMC). At least at UWMC, we don’t have to drive deep into Seattle – just across the lake.
The most disturbing thing about these visits, though, was that the doctors acted as if the treatment was just a foregone conclusion: but of course, we would want to do radiation and chemotherapy. Why would we not? I think these discussions were more difficult for Laura than going through the surgery was. She has lived her life in a healthy way so as to avoid putting anything toxic into her body, and here were the professionals telling her to do just that in order to deal with this cancer.
<rant>
There: I said the “c” word. I hate using it – people react to it and most usually don’t know how to respond or treat you, and in many cases, they start avoiding you. I was told, and I understand it now, that it is not that they don’t want anything to do with you but just don’t know what to do and how to treat you; that they retreat and think they don’t want to be insensitive or be a burden to you. I will say, though, that the best way to treat someone who just told you they have cancer is to treat them like you did before. Don’t change on their behalf, don’t “back off” to give them space. Still ask for their help, still ask them to do things, still ask to spend time with them. Make sure they feel valuable to you and not a waste of space.
</rant>
Following up after the meetings, the “care team”, as the team of doctors and nurses is called, had realized that Laura had not had a post-operative MRI done, so on December 16th, we went in for an MRI and what they called a “planning” CT. The CT combined with the new MRI would be a 3D map of the area to be treated so that radiation could be targeted to a specific area.

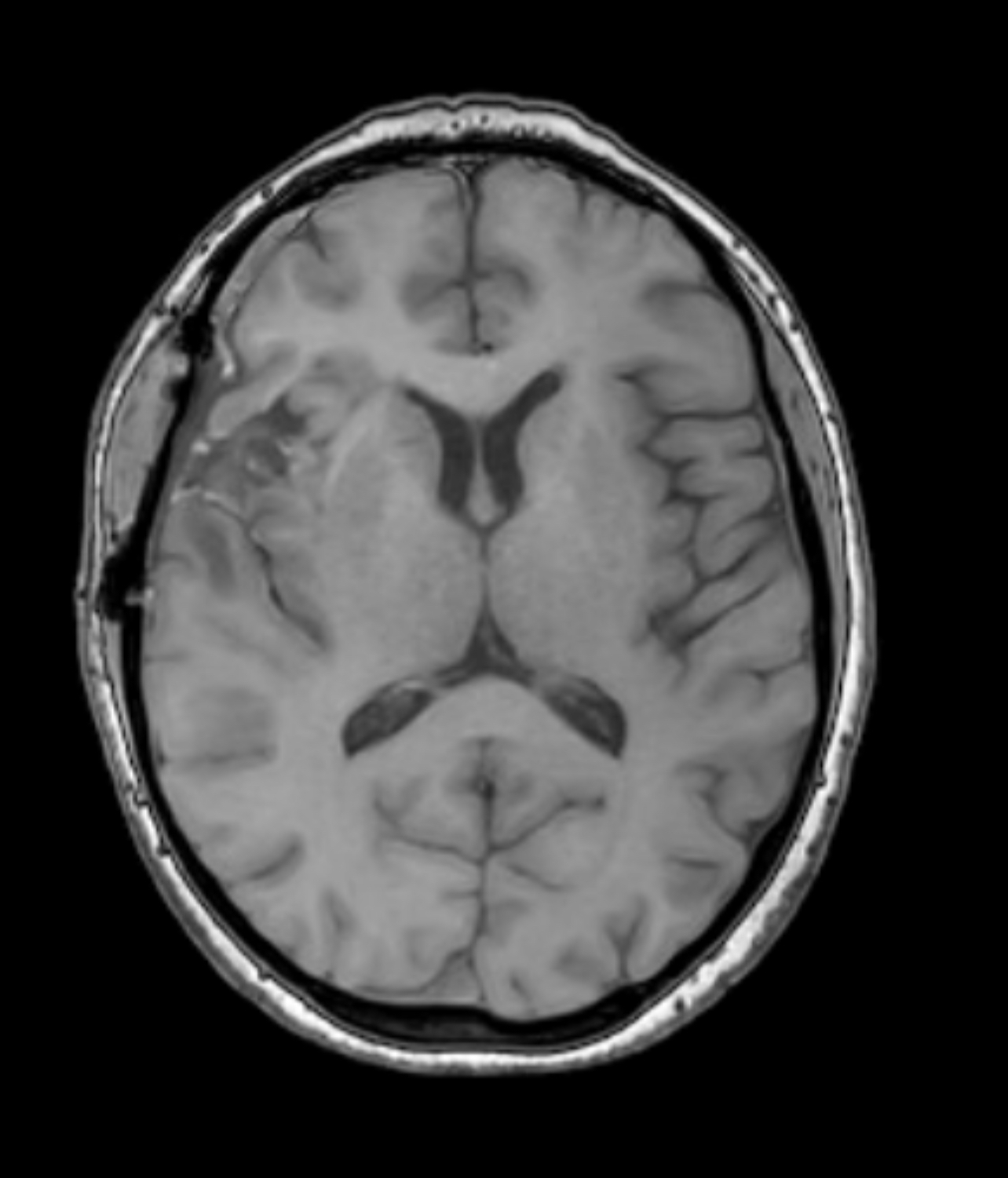
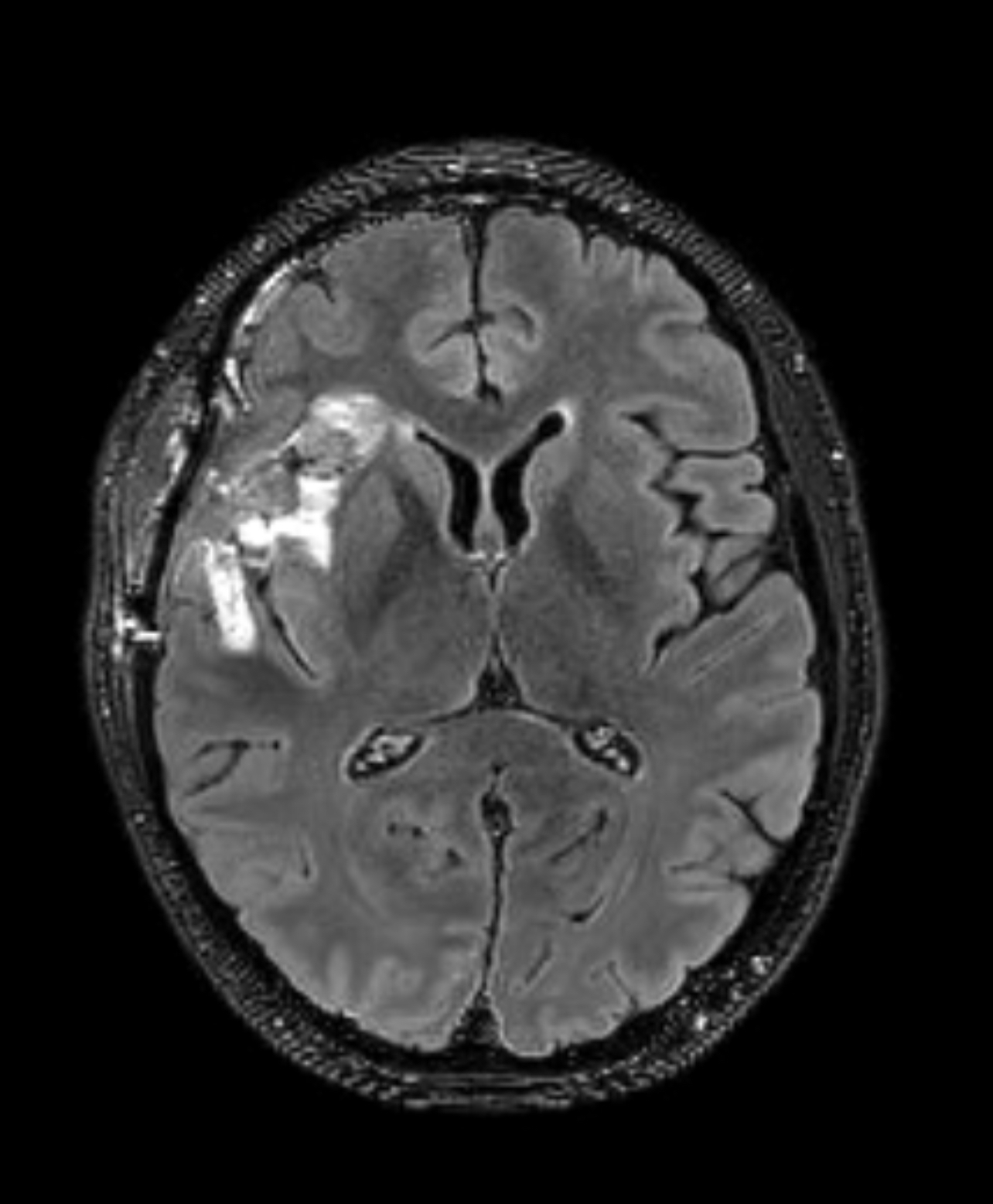
These images are backwards: left is right, right is left. Our doctor is looking at the before and after images in the first one, but the scans on the right are the new MRI scans (without contrast and with contrast). Notice how much healthier her brain looks a month after surgery! The part of concern is the bright area on the picture in the far right. That is the section where the tumor was removed from and where there may be some remaining cancer cells. Of course, it could also just be inflammation – they were a little unclear on that.
The plan is to continue the radiation and chemotherapies for a “cycle”, let the brain chill out for a couple of months, and then do another MRI to check the progress… and another and another. They want to keep doing MRIs to make sure nothing grows back after the treatments, because it is the only way to know if it’s gone. Remember the blood-brain barrier? Well, that means there is no blood test with this kind of cancer – they have to keep looking. So, the scans will go on for a while.
And speaking of “plan”, in order to get set up for treatment, following the MRI, the did a “planning” CT to complete some 3D mapping of the treatment area which required Laura to get a mask device created to hold her head is a precise location and position.
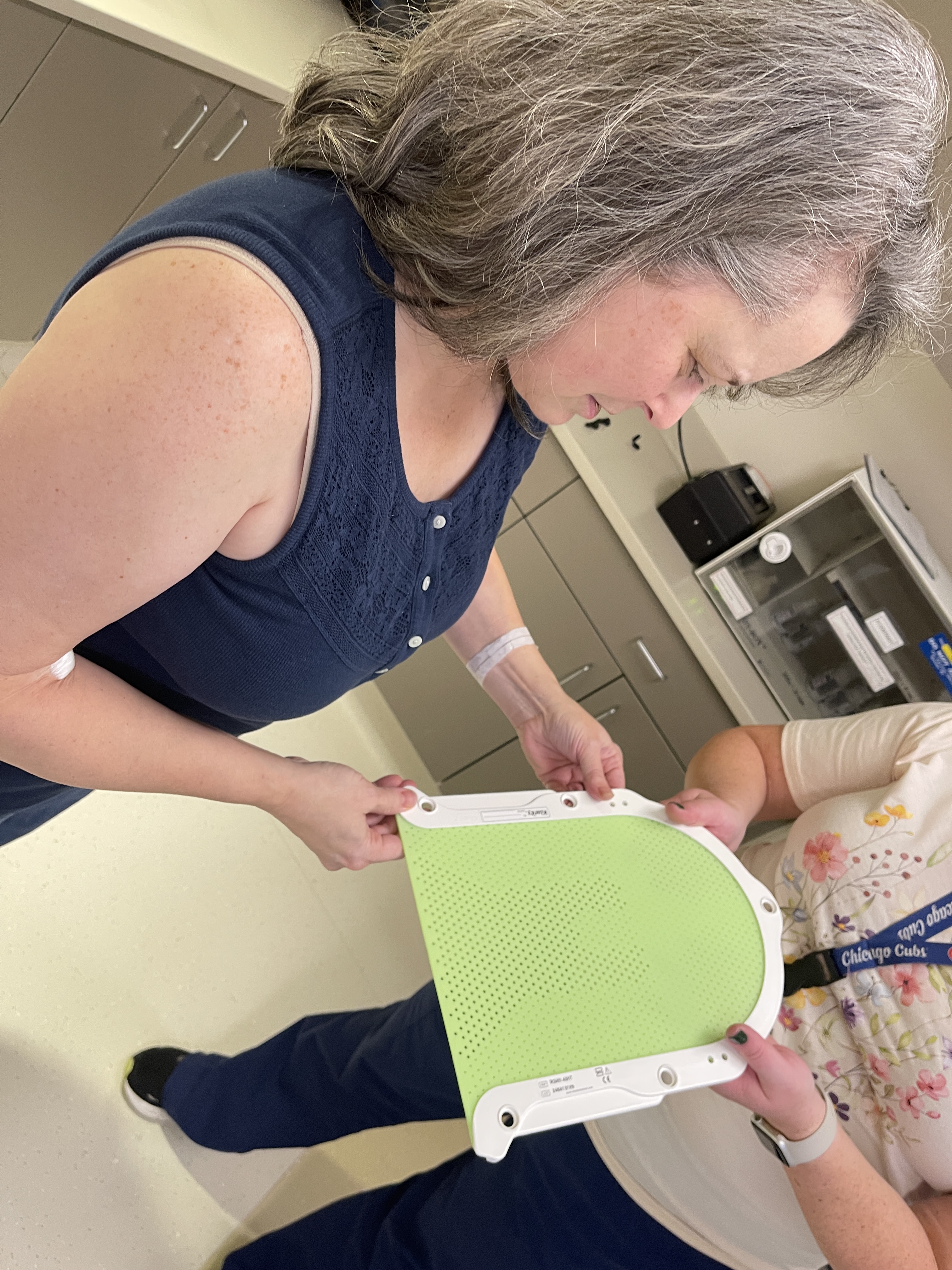
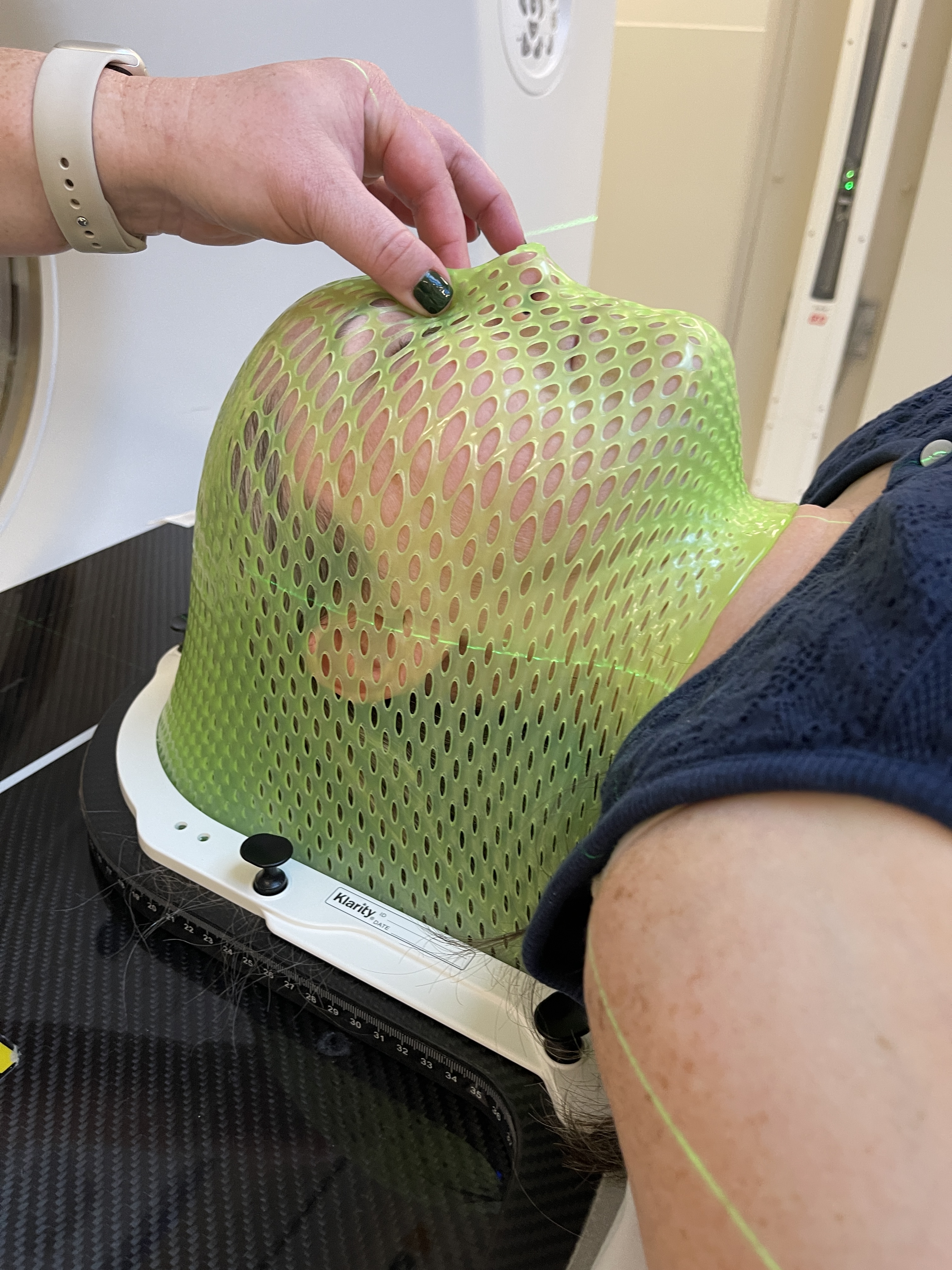

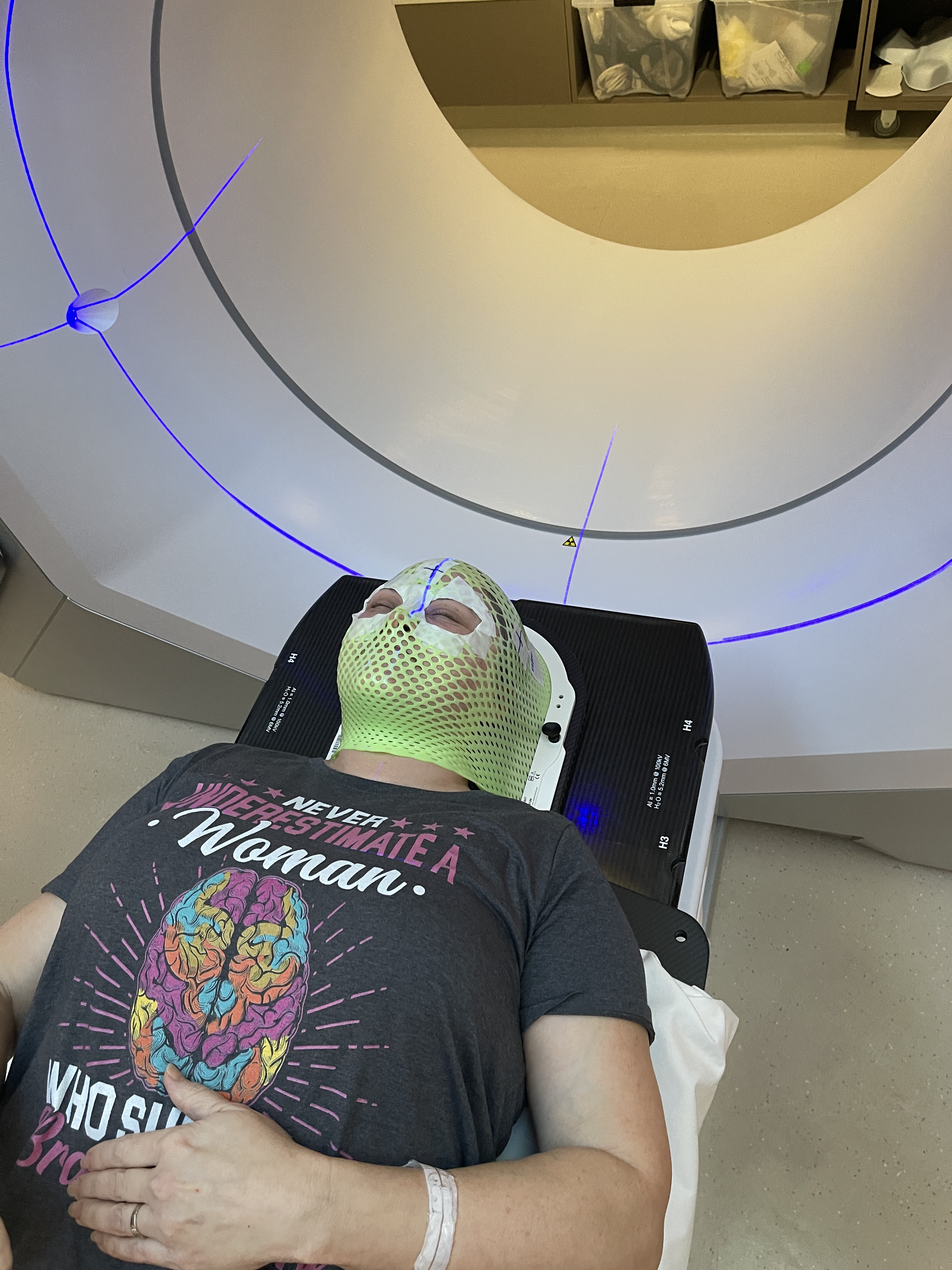

The first two pictures are of the mask creation on December 16th. The last 3 pictures are of a treatment day with Laura climbing onto the machine and getting “masked up”. The last picture is a quick shot of the treatment plan with some 3D imaging and target area mapping. We made them show it to us at one of the follow up visits.
While the radiation was getting planned out and scheduled, we were supposed to be getting her chemotherapy medication – not the intravenous type, thank God! It is in pill form and a much milder version, which is targeted specifically for this type of tumor. However, it is a specialized drug and not found at most pharmacies. We had to order it from a specialized online pharmacy. This was supposed to happen through my old job’s insurance claim process in the end of December. Unfortunately, they drug (ha) their feet long enough that my insurance expired while we were waiting for a call back and we had to re-initiate the process of getting it approved and ordered on the new insurance with yet another online pharmacy.
While these two things were supposed to happen simultaneously, we ended up having about a 3-week delay in getting the medication. So, Laura ended up getting a bit of a break from the double whammy of radiation and chemo meds and was able to ramp up a little more gently with radiation first, followed by chemo a couple weeks later.
It was still a major pain to deal with. And yes, that picture at the beginning of the post that says “hazardous drug” is the package it came in.
As of now, we are in the beginning of the sixth and final week of radiation treatment and that means it should wrap up in just under one week from today. Laura will be glad that it is done. That will also mean that she doesn’t have to get up so early each day – although, it’s been somewhat motivating for her to have that schedule. Both the chemo and the radiation will stop at the same time, giving her a break to recover her strength and to detox from the drugs.
We are so ready for this part to be over.

One thought on “The Unexpected Journey – Part 6: Treatment”