After the whirlwind stressful day of surgery, I was not really able to sleep well at all. If any of you have stayed in a hospital, you know that the nurses are masochists and love to make you sleep deprived. Yes, I know it’s their job to make sure the patient is alive and well, but waking people up every 3 hours after they JUST got to sleep is, well, mean. In spite of that, I have to say that our nursing team were all wonderful people.
Not that I was really asleep anyway. I could not relax after the surgery, partly from relief, partly from joy that she was out and still alive, and partly because I was also just too tired to sleep. Or maybe it had something to do with the coffee.

The sleeper sofa was wide and solid, but a little hard. It was a nice touch, though.
Laura at this point was itching to get up, sit up, walk around, and just do things in general. She had been laid out with pain for so long, that the absence of it was making her want to start doing things.
Of course, major surgery can take a lot out of a person, so she was also sleeping quite a lot – but only in small bursts, since she kept getting woken up for “vitals” checks.
After the first day, the change in Laura’s alertness and awareness was amazing. She was recovering faster than anyone thought she would. Before surgery, the tumor was pressing her brain so hard, that not only did it hurt constantly, but she was even unable to think clearly. Now that it was gone, she started doing and thinking more a little at a time. To me, the change was remarkable, and she was on her way back. To the doctors who came by periodically to check on her, she was doing amazingly well.
DO NOT PANIC – These are good news scans below:
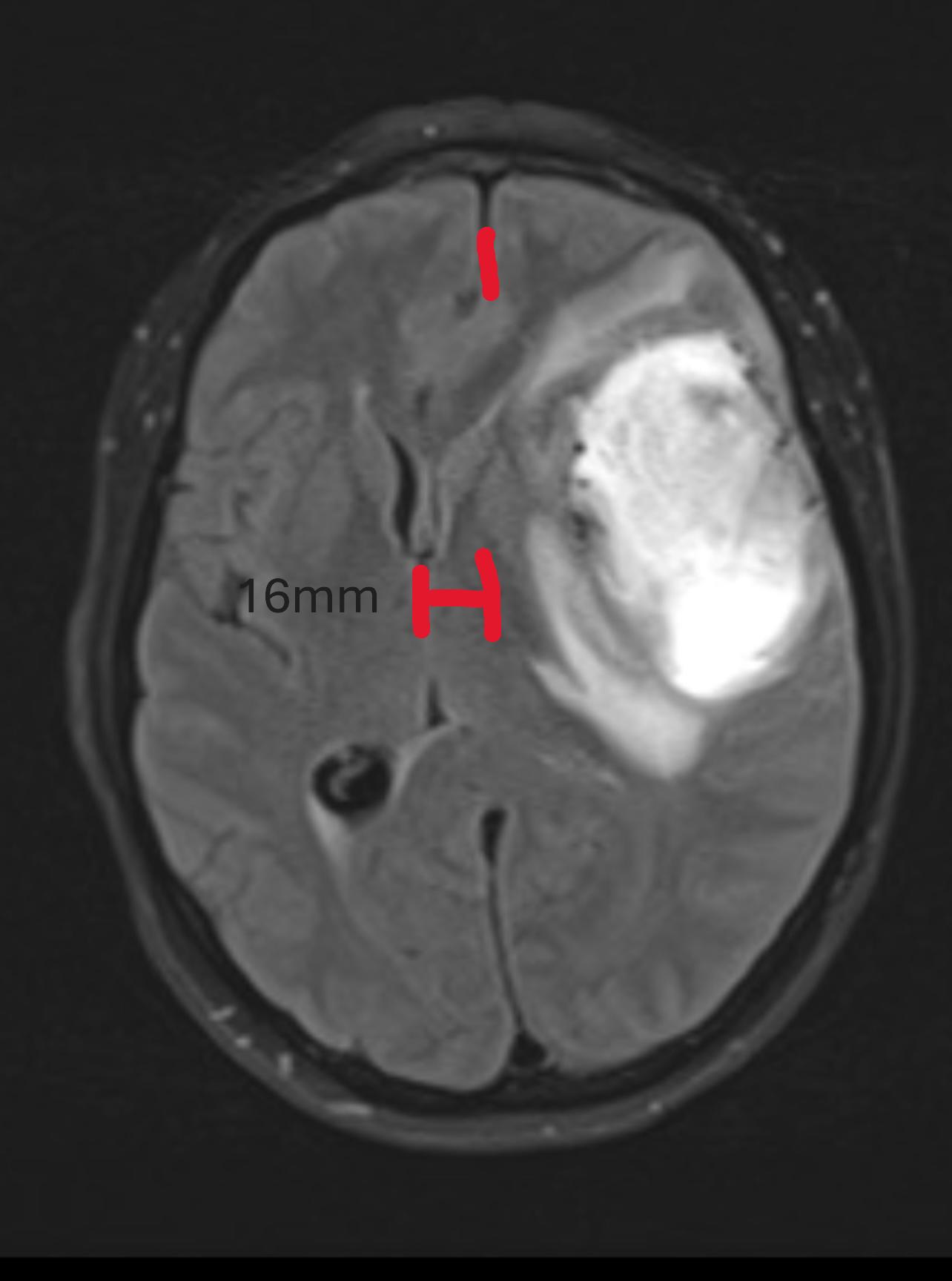
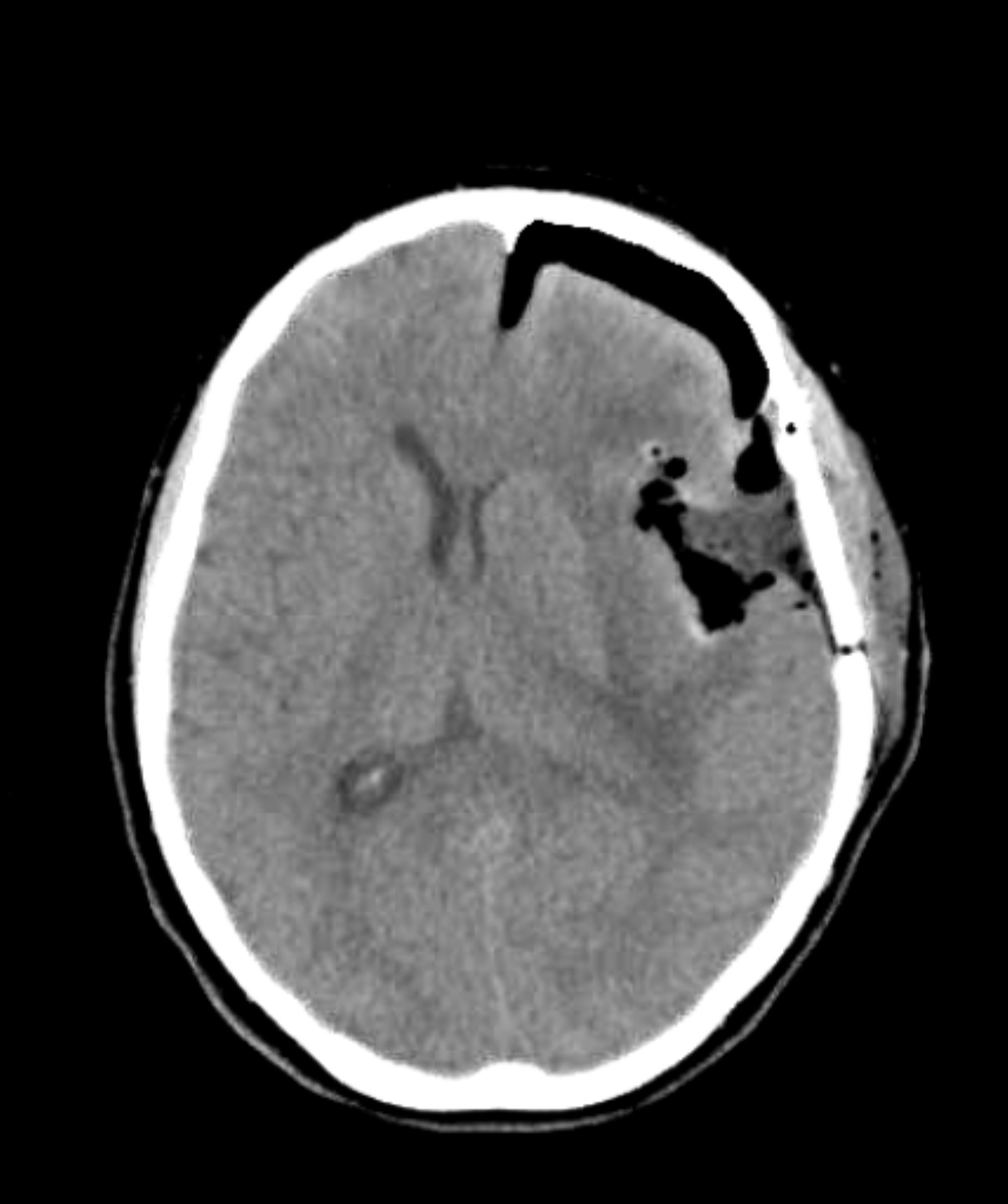
The neurosurgeon came to show us the CT scan for the after-surgery look at the place where the tumor used to be. The before is on the left, and the after on the right. They look different because the before is an MRI and the after is a CT scan, so they have different resolution and contrasts. The white area on the before is the tumor. On the after shot, you can see a lot of black areas: those are air gaps where the tumor no longer exists. You can even see the gap between her skull and brain to see how much extra space the tumor was taking up. This picture was taken immediately after surgery, but even so soon after surgery, the midline had moved over half the distance it was displaced by (now only 8mm), and the brain had begun re-expanding since the pressure was no longer there. HUGE improvement! No more headaches!

Those flowers are on a wall mural in the NeST area, and you can see that Laura is much happier walking around outside of the room. They would not take out the IV plugs “just in case” while she was there. Those were bothersome for her until the day of release.
That night, 24 hours after surgery, Laura wanted to wash her hair – but, with the incision and the sealant on her scalp, she had to be very careful. Luckily, nurse Madie was able to help her do her hair properly without causing damage to the incision area.
The next day (Friday), after several visits from doctors, therapists, and nurses, we were told that Laura was doing so much better: that they expected people who had been post-op for 3 weeks to be doing as well as she was doing only 2 days after surgery. The recovery was going spectacularly. So well, in fact, that Laura was given a “hall pass” to wander around the entire hospital – just not allowed to leave yet. They have an outdoor observation deck/lounge that we were supposed to go to, so we suited up with jackets and sunglasses ready for the sun.


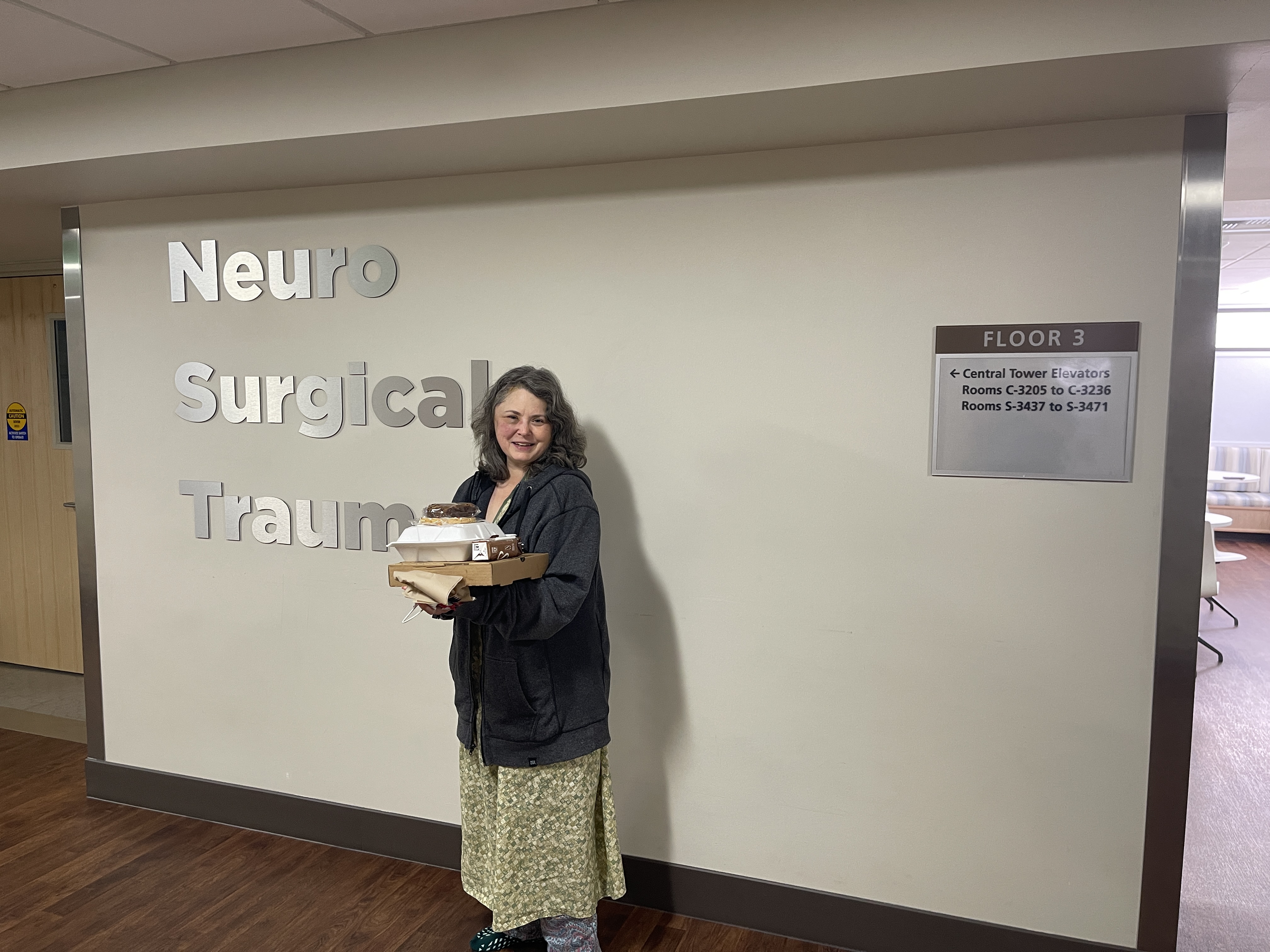
Unfortunately, the deck ended up being closed for the season just the day before. We then proceeded to wander around the building, stopping at the gift shop and finding a place where the view of the mountains was the best. Laura was disappointed that the selection of T-Shirts at the gift shop did not include any post-surgery “victory” shirts. She would later rectify the situation with orders from Etsy.
Once we got back, we met the oncology doctors in the NeST hallway – they were looking for us. We had never met them, but I could tell from their expressions that they were the “bad news” doctors. What they told us shouldn’t have been a surprise for us, I suppose, but it wasn’t something that we really had thought through. With the resounding success of the surgery and the clear relief from pain, we didn’t think too far past that.
What they told us was that the tumor was something called a glioblastoma. At the time, we had never heard of this. Apparently, there are things called “glial” cells which support the neurons in the brain and that is where this tumor grew – right on the outside edge of the brain. Good for us since it could be removed easily, instead of some tumors that grow deeper inside. More tests were still to be done to determine the type of glioblastoma and its grade. Brain tumors inside the blood-brain barrier do not have “stages”, but “grades” because they do not spread outside of the brain. Other cancers in the rest of the body are classified in stages, because they can spread to other areas or “metastasize”. Most brain tumors do not do that.
The implications of that, however, meant that they were referring us to a cancer treatment center in our local area. If I had to deliver news like that frequently, I would also have a sad expression on my face most of the time.
The shock of this was somewhat mitigated by the fact that the final test results were a few weeks off, and by the fact that God had gifted us with a wonderful care team in a great hospital, and that He had also given us joy to be alive and together. It was almost like a vacation – if on a vacation you go scuba diving, get the bends, have to go to a decompression chamber, and get treated for a shark bite while you’re at it, but still get to be on the beach.
Even that news couldn’t keep us down for long. We knew that we were close to being discharged and that we would be coming home soon.
Plus, we were facing this together. Always.

What an amazing change so quickly after surgery! Go, Laura! WooHoo!
LikeLike